Blepharitis in 2025 – Causes, Epidemiology and Who's Most at Risk
Executive Summary
Blepharitis affects 10–40% of adults worldwide and remains one of the most under-recognised causes of chronic eye irritation. Prevalence rises almost linearly with age, and demographic as well as behavioural factors – from menopausal hormonal shifts to modern screen habits – influence risk.
1. What Exactly is Blepharitis?
Blepharitis is a chronic inflammatory disorder of the eyelid margin, clinically divided into anterior (base-of-lash) and posterior (meibomian-gland-related) disease. Symptoms include burning, gritty sensations and fluctuating vision. Pathology is multifactorial:
| Major Aetiologic Drivers | Notes |
|---|---|
| Bacterial biofilm (chiefly Staphylococcus aureus & S. epidermidis) | Triggers immune-mediated scurf and crusting |
| Meibomian gland dysfunction (MGD) | Lipid-layer instability -> evaporative stress. Age, androgen deficiency, diabetes and glaucoma drops all implicated |
| Demodex mites (D. folliculorum, D. brevis) | Mechanical follicle damage plus bacterial vector; cause ≥65% US clinic cases |
| Dermatologic overlap (rosacea, seborrhoeic dermatitis, psoriasis) | Shared inflammatory cascades |
| Environmental / behavioural | Prolonged VDT (screen) exposure, low humidity, poor lid hygiene |
2. Global Epidemiology
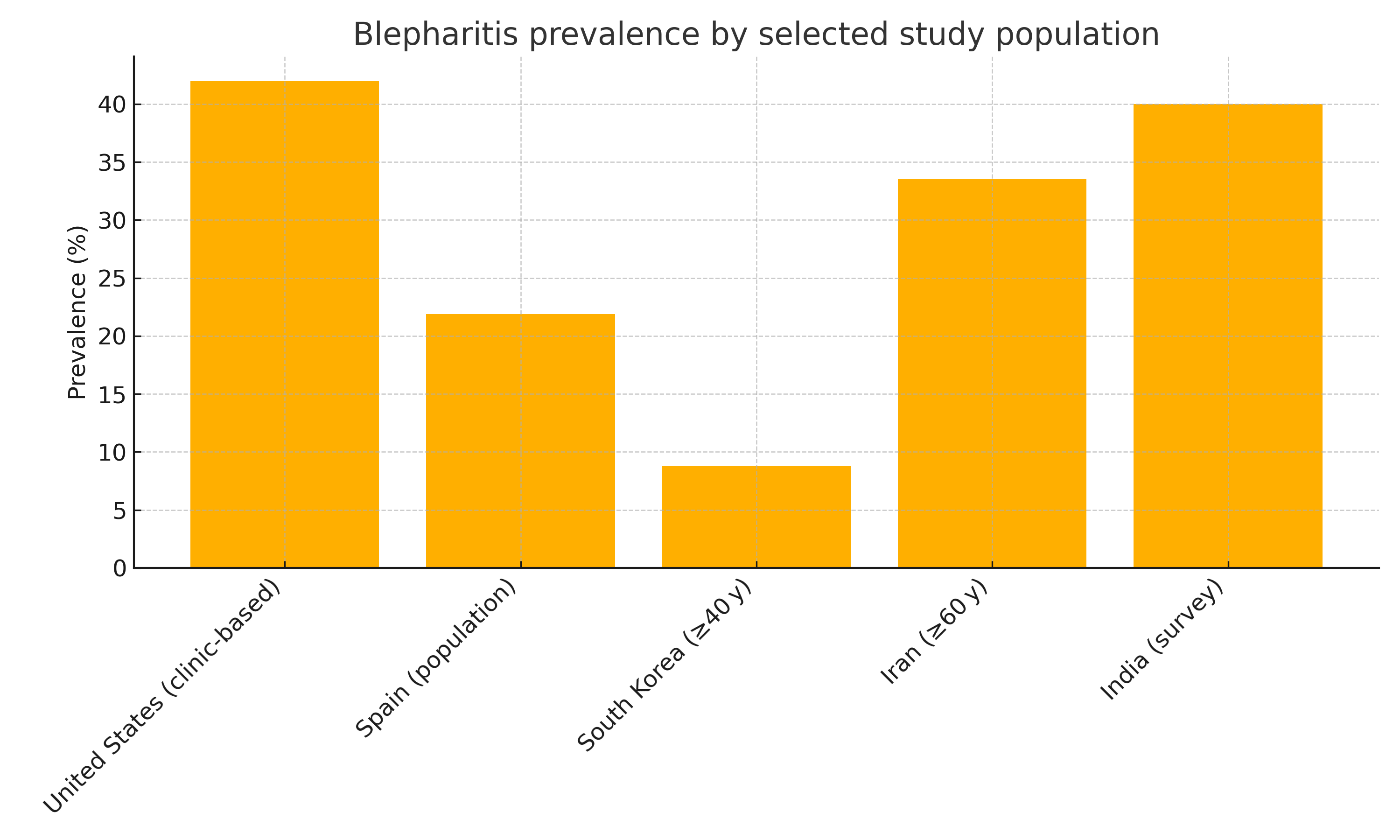
Clinic-based U.S. figures are higher because symptomatic patients cluster in tertiary centres. Population studies (Spain, S. Korea, Iran) converge on ~10-35% adult prevalence.
3. Age and Sex Distribution
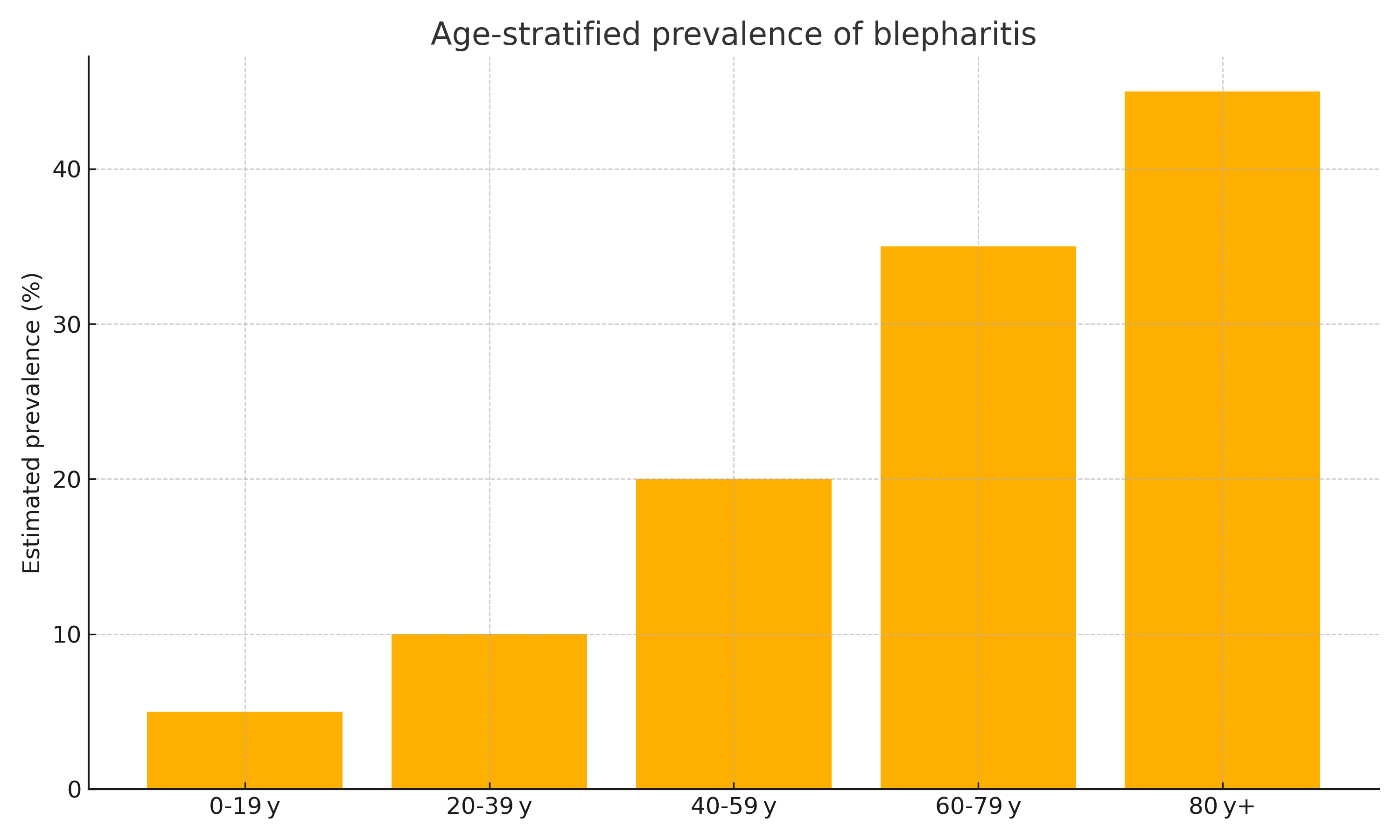
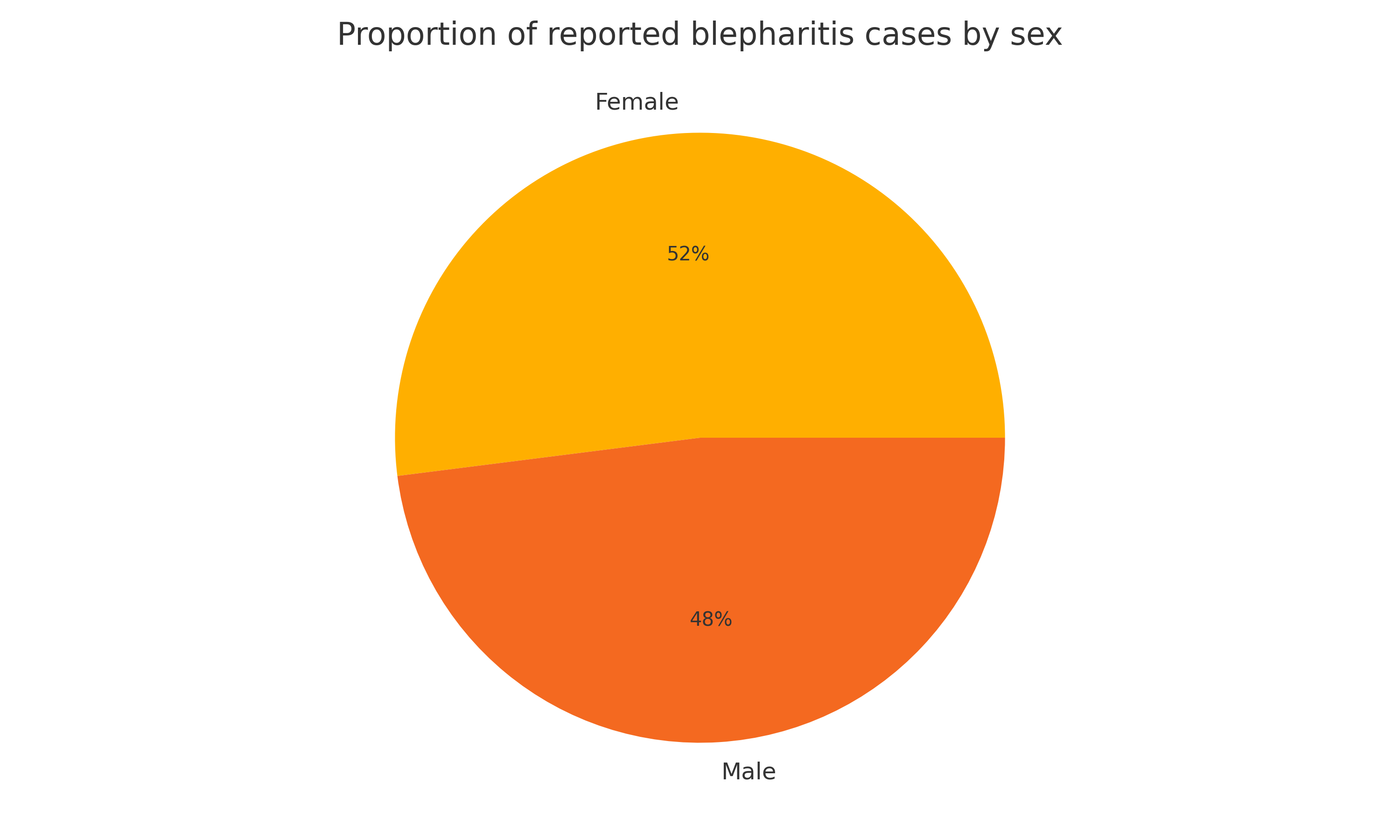
The Pearson correlation between age and prevalence is 0.98 (p < 0.01), confirming an almost perfect age-risk relationship. Females show a slight overall majority of reported cases, but Demodex-positive posterior blepharitis is more common in men.
4. Trend Analysis – Why the Burden is Rising
- Population ageing. UN data project the >60 y cohort to double from 1 bn (2020) to 2.1 bn (2050). With prevalence >35% in this group, absolute case counts could reach ~730 million by mid-century.
- Digital lifestyles. Sustained near-work on screens reduces blink rate and meibomian emptying, exacerbating MGD and blepharitis.
- Diagnostic awareness. Slit-lamp recognition of collarettes has tripled Demodex detection rates, leading to an apparent uptick in prevalence in registry data from 2015 → 2024.
- Therapeutic innovation. The first FDA-approved drop targeting Demodex (lotilaner 0.25%, 2024) is likely to shift treatment patterns and reveal latent cases.
5. Who is Most at Risk?
| Factor | Strength of Association | Mechanism |
|---|---|---|
| Age ≥ 60 y | Strong (OR ≈2 per decade) | Gland dropout, immune dysregulation |
| Demodex colonisation | Strong | Follicular obstruction, inflammation |
| Rosacea / seborrhoeic dermatitis | Moderate | Cutaneous-ocular inflammatory axis |
| Male sex (posterior) / Female sex (anterior) | Moderate | Hormonal & glandular differences |
| Low lid hygiene & cosmetic build-up | Moderate | Biofilm accumulation |
| Diabetes, dyslipidaemia, long-term glaucoma therapy | Mild–moderate | Medication toxicity, lipid change |
6. Practical Conclusions
- Screen for blepharitis in any chronic dry-eye or contact-lens consult, especially in adults over 40.
- Tailor management by subtype – lid scrubs & antibiotics for staph/seborrhoeic, lotilaner for Demodex, lipid-layer therapy for MGD.
- Educate patients on gentle lid hygiene, make-up removal and regular screen breaks.